Manual Therapy Online - Articles
Vertebrobasilar Insufficiency Article #3: Dizziness
In the first essay, “VBI: the 5 Ds” I argued that using the 5Ds as a group identifier of the presence of vertebrobasilar ischemia was useless and in fact dangerous for a number of reasons. I argued from available evidence that first most of the symptoms were not commonly associated with traumatic VBI and that the second most common symptom headache was not included in the 5Ds because it had the misfortune to start with “H”. The exceptions were dizziness and dysarthia one of which we will discuss in this essay. My second argument was that most commonly there were no clear neurological symptoms at the onset of VB stroke let alone the transient syndrome that would likely occur with our patients. For these reasons the 5Ds as a group or individually are neither useful as a screening protocol nor as a diagnostic tool as they are neither sensitive (unless dizziness as a single symptom is used, in which case it is too sensitive) or specific for VBI.
This essay will look at the most common symptom of VBI, dizziness and how to start to gain an appreciation of how indicative it is of a serious central neurological problem and how it can be used together with the presence of headache and neck pain to make a presumptive diagnosis of VBI and avoid moving the patient’s neck at all.
Dizziness is probably best defined as a sense of disequilibrium and it can include; vertigo, oscillopsia, giddiness, wooziness, nausea, vomiting, light-headedness and almost anything else the patient is pleased to call dizziness. This feeling of disequilibrium can be caused by problems in the organs responsible for sensing imbalance, the peripheral nervous system taking the sensations to the central nervous system and the central nervous system components that process the information. It can also be caused by visual and other inputs that impair the perceptions of balance such as when a train slowly pulls out of a station so that it appears as if the station is moving and leaving the passenger with a very weird feeling that can be described as dizziness. Another example is motion sickness.
The term therefore requires categorization and the usual classification of dizziness is peripheral and central. Central dizziness can defined as dizziness caused by impairment of the central neurological system that deals with balance (that is the perception perturbations in the center of gravity and the volitional and reflexive responses to such perturbations) while peripheral dizziness is, for the most part, caused by dysfunctional sensory organs of balance.
Central balance structures include the vestibular nuclei, the vestibular tracts, thalamus, cerebellum and neocortex while peripheral structures include proprioceptive receptors in the extra-ocular muscles, the TMJ and its muscles, the entire spine and limbs, the trunk muscles and even the pressure receptors on the soles of the feet. But probably the biggest influence on the sensation of dizziness are from the tissues closest to the head that is the eyes (vision and proprioception from the muscles) and the upper neck and to a lesser extent the TMJ.
This classification of peripheral or central dizziness is an etiological classification but has to be established from assessing the patient’s dizziness so the precursor of the etiological diagnosis must be a symptom based classification and this is classifying dizziness into either Type 1, Type 2 or Type 3.
Type 1 dizziness is an illusion of movement, either vertigo (a spinning movement) or oscillopsia (a swaying or linear movement).
Type 2: is termed pre-syncope dizziness after the feeling that you are going to pass out and includes all forms of dizziness sensations that are not Type 1 such as giddiness, light-headedness, nausea etc.
Type 3: this really isn’t dizziness as defined above but actually imbalance or disequilibrium.
So if we take the example of what happens when you spin around and around, the first sensation is Type 1 followed by the regret that you did it caused by Type 1 and during the Type 1 dizziness Type 3 occurs as you stagger around trying to find you center. By comparing the patient’s symptomatology with the illness scripts of peripheral and central dizziness we can start to make a clinical determination of the etiology of the dizziness and take the appropriate steps; either refer out for more definitive diagnostic measures or continue with the examination.
Type 3 dizziness unassociated with Type 1 dizziness should be considered part of a neurological impairment, degeneration of or disease/injury to the central nervous system such as the cerebellum. When it is associated with Type 1 dizziness the problem may be of either central or peripheral origin.
Type 1 dizziness perhaps allows us the clearest determination as to whether the dizziness is due to central or peripheral lesions. By far the commonest for that Type 1 dizziness takes is vertigo and its most common direction is around a vertical axis if upright or a coronal axis if lying. However, it can be around a sagittal axis so that the patient feels he/she is somersaulting forwards or backwards and this is so unusual that you should probably consider the cause to be central.
The table below outlines the similarities and the differences in the type and behavior of the vertigo.
| Labyrinthine | Central | |
| Intensity | Severe | Moderate (VBI may be severe) |
| Persistence | Non-persistent | Persistent (VBI 20mins-20 hrs |
| Axis | Vertical sometimes coronal | Vertical may be sagittal |
| Direction consistence | Consistent | May alternate |
| Neurological symptoms | None (may have blurred vision) | May be but with VBI usually not |
| Neurological signs | Nystagmus (appropriate for VOR disturbance0 | May have variable signs mostly related to lateral medullary syndrome) |
Type 2 dizziness is much less clear in pretty much all respects. There is no clear operational definition as there is with Type 1 and it may include any of the following and more besides:
- Wooziness
- Giddiness
- Light-headedness
- Nausea
- Vomiting
- Unsteadiness
- Faintness
- Weird feeling
- Etc.
In fact, anything that the patient relates as dizziness is dizziness. Additionally, the intensity and timelines that were present for Type 1 do not obtain for Type 2. But severe dizziness and prolonged persistence may indicate more serious causes. Anything lasting more than 15-20 minutes should be viewed with suspicion especially if it is not improving or is worsening. This is where a neurological examination becomes essential and at a minimum a cranial nerve exam should be carried out and if positive the patient must be transported to the emergency room.
Causes of Dizziness
These are multiple and extensive.
- Middle and inner ear problems including Meniere’s disease, viral infection, acoustic neuropathy, canalolithiasis/cupulolithiasis (BBPV), labyrinthine concussion (temporal bone fracture, traumatic hydrops, fracture/dislocation of the oscicles, rupture of the tympanic membrane, and oval window), middle and inner ear infections,
- Migraine
- Circulatory problems including orthostatic hypotension, cardiac arrhythmias, myopathy, failure and attacks.
- Neurological conditions such as MS can lead to progressive loss of balance.
- Cerebellar pontine tumors
- Metabolic disorder including anemia and hypoglycemia
- Medications. There is something like 400 drugs listed as having dizziness as an adverse effect including most of those our patients are taking such as NSAIDs, analgesics.
- Age. Older patients are more likely to have problems with balance and the attending sense of disequilibrium due partly to degenerative changes but also because of the higher likelihood of developing a medical condition that causes dizziness.
- Pretty much never mentioned in the literature but well known to us is spondylogenic dizziness caused by a conflict in messages between the components of balance from cervical dysfunction.
So the pathologies that will mainly concern us are in this essay are:
- Traumatic VBI
- Vestibular dysfunction
- Spondylogenic dysfunction
It would appear from the literature that dizziness is somewhere between 95-100% sensitive for traumatic VBI and that the dizziness may be either Type 1 or Type 2. Type 1 dizziness can usually be fairly easily classified as central or peripheral but regardless of that it does need to be evaluated by a specialist in the area.
As with most things basing a diagnosis on a single symptom is not the best idea except where that symptom is pathognomonic of the condition so it is very necessary that other symptoms and tests are integrated into the process. But, some of these tests may well be dangerous if the patient is suffering from VBI and it may well be that the subjective examination will contraindicate any movement testing of the patient. This applies particularly to those conditions where movement could be disastrous; especially VBI and high cervical fracture. So be wary of the following:
- Sudden traumatic onset of severe occipital pain and dizziness
- Central vertigo
- Sagittal plane vertigo (somersaulting)
- Prolonged or severe Type 2 dizziness
- Progressive dizziness
- Dizziness and blurred vision
In all of these cases it would probably be best if movement tests (the so-called vertebral artery tests and ROM tests) be avoided. A cranial nerve examination (CNX) while the patient is dizzy if possible is the best approach but if the patient is not dizzy or if the CNX is negative integrate the behavior of the dizziness with the behavior of the headache and neck pain to associate or disassociate the symptoms (covered in a later essay).
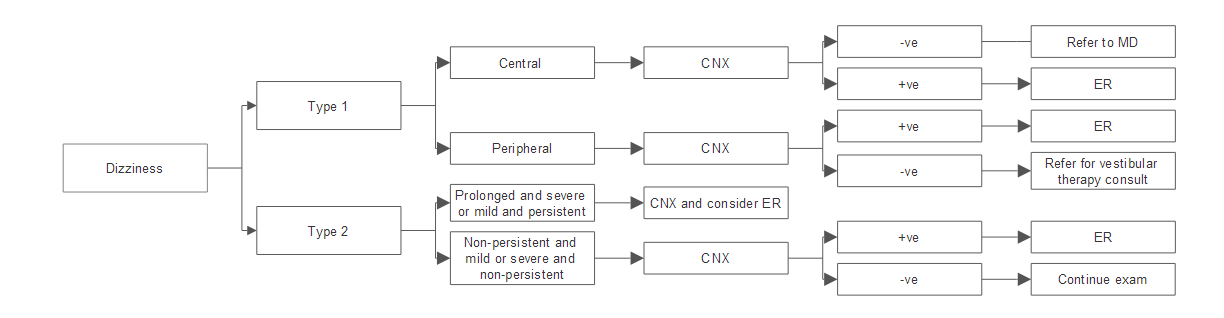
The following flowchart is a suggestion on how to deal with the subjective aspect of dizziness in isolation of other subjective questions or physical tests except for the CNX. Of course in the clinic the examination is not isolated to dizziness but includes its relationships with neck pain, headache and the results of other physical tests. These aspects will be dealt with in another essay but I would suggest that regardless of the results of these tests pan out the patient I have recommended go to the ER should go to the ER.
Next essay on VBI is about headaches.
comments powered by DisqusFeatured Course
FREE COURSE
Foundations of Expertise
Date:
Starting March 24, 2024
Location: Online
LEARN MORE



